Sunday, March 28, 2021
Alex Papp, MD
Joe is in his mid-fifties, an accomplished attorney who has been suffering from recurrent depression since his early adulthood. The depression was difficult to treat; many different medications have been tried, including mood stabilizers (medications for bipolar disorder), but those were prescribed such a long time ago that Joe had a hard time remembering how he was feeling when they were prescribed. All he knew that for at least the last ten years he was only depressed, sometimes more, sometimes less, but never free from it.
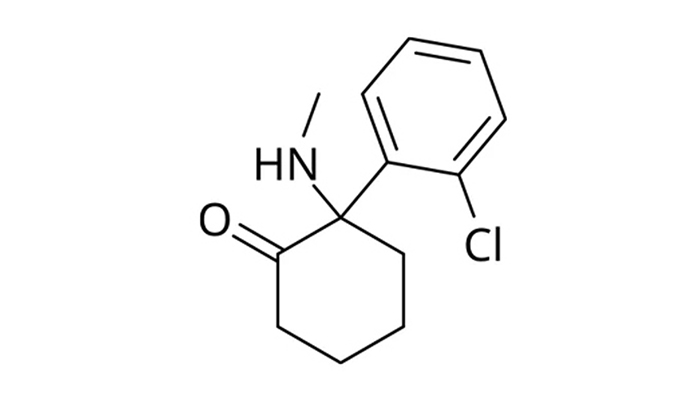
He was one of the first patients I treated with Ketamine, originally in a different setting. He was under the care of another psychiatrist who continued to prescribe his 20 mg Trintellix, the antidepressant Joe had been taking for many years. This “split” treatment is standard practice at the so-called Ketamine Clinics, and is available at PLC as well, as an option.
His mood improved partially, but noticeably more than during ten years of taking the antidepressant tablet alone. It became easier for Joe to complete tasks, which allowed him to increase his activities in business and eventually develop a romantic relationship, but many less important activities, such as fixing broken items at home, remained undone.
He settled into a pattern of monthly ketamine visits at PLC and trimonthly visits with his psychiatrist. At one point the psychiatrist retired and Joe elected to consolidate both the traditional medication treatment and the Ketamine treatment at PLC.
The first sign that something was changing was him beginning to report irritability. He lashed out at meetings at work, which eventually resulted in him losing one of his important clients. He told me that he used to have that problem many years ago, probably before his depression became severe. He admitted that he was having a difficult time controlling these outbursts but initially he denied that they constituted a problem.
During subsequent treatments we spent more and more time discussing this issue. At the second-to-last visit, when it became clear that this behavior continued to worsen, and he started to have some difficultly falling asleep, we embarked on a slow tapering off the Trintellix.
When he showed up for his most recent visit, Joe was taking it every other day, at an effective daily dose of 10 mg only. It was clear, however, that Joe was in a “hypomanic” state: he was talkative, his mind was racing, he was even more irritable than before, among many other symptoms of that condition.
I informed Joe that Ketamine was no longer indicated since he was no longer depressed. He was a bit surprised and disappointed, but he understood the reasoning. He even admitted that he himself knew he became hypomanic.
At this point his diagnosis had to be changed from “Chronic Depression, questionable Bipolar Disorder” to “Bipolar Disorder”. His psychiatric treatment at PLC will continue in a more traditional fashion, focused on the new diagnosis. If his depression returns in the future, and it again fails to improve with treatment, Ketamine may be indicated again.
We at PLC believe that one of the advantages of Ketamine being administered in a general psychiatric practice is that it is easy to catch changes in the clinical presentation, changes that may necessitate reevaluating the feasibility of the Ketamine treatment on the spot. I wonder how long it would have taken to notice Joe’s change from depression to hypomania in a setting where he gets Ketamine at a Ketamine Clinic, while seeing a general psychiatrist, or perhaps even only a primary care physician, every 3 – 6 months elsewhere. Chances are that it could have taken several visits for something to start looking suspicious. Joe himself was ready to go along with the treatment, having settled into the chair as usual, and only careful discussion reveled that things have become very different.