Wednesday, May 01, 2024
Alexander Papp, MD and Julie Myers, PsyD, MSCP
Treatment-resistant depression (TRD) is a complex challenge in mental health, characterized by patients’ inadequate response to standard antidepressant therapies. The landmark STAR*D study, which extensively evaluated treatment strategies for depression, revealed that a significant percentage of individuals do not respond to traditional antidepressants even after several attempts and varying approaches. This study importantly suggests that previous treatments may have been insufficiently applied, in terms of either medication dosage or duration, before considering a diagnosis of TRD (Rush et al., 2006).
TRD may also be influenced by underlying physical or other mental health conditions, which can complicate or mask the typical presentation of depression. Conditions such as thyroid disorders, chronic pain, or co-occurring anxiety disorders can alter the efficacy of conventional treatments and may require a different therapeutic approach. This complex interplay underscores the necessity of a comprehensive assessment by a trained psychiatrist, who can evaluate the full spectrum of factors contributing to each patient’s unique case and adjust treatment plans accordingly.
Advancements in genetic testing are playing an increasingly vital role in addressing TRD. Pharmacogenomics, the study of how genes affect a person’s response to drugs, can significantly enhance the personalization of treatment. By identifying genetic markers that predict how patients metabolize certain medications or respond to specific treatments, psychiatrists can tailor therapies that are more likely to be effective and have fewer side effects, potentially shortening the trial-and-error process often associated with the treatment of depression (Porcelli et al., 2011).
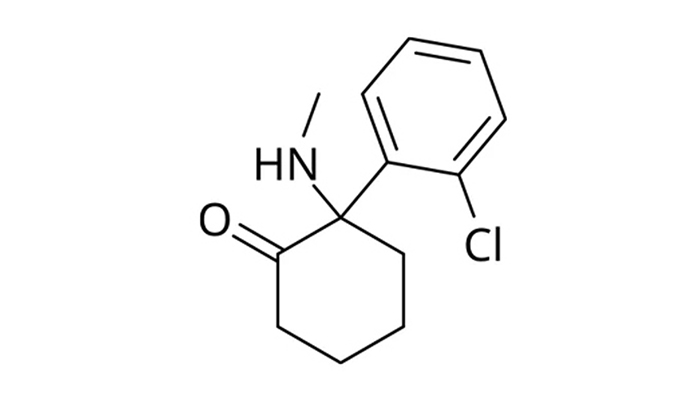
Innovation in pharmacotherapy offers new hope for those with TRD, with emerging drugs and alternative medications such as psychedelics gaining attention for their potential benefits. Substances like ketamine and psilocybin are being explored for their rapid-acting antidepressant properties and ability to target different neurobiological pathways than those affected by traditional antidepressants. However, the use of these treatments involves careful clinical consideration and should only be conducted under rigorous psychiatric supervision to ensure safety and efficacy. This tailored approach highlights the critical role of psychiatrists in the management of TRD, ensuring that all potential treatments are considered and appropriately administered (Davis et al., 2020).
Summary
- Influencing Factors: Treatment Resistant Depression (TRD) can be affected by physical or mental health issues like thyroid disorders or anxiety, which might necessitate alternative treatments.
- Complexity of TRD: Treatment-resistant depression often does not respond to standard therapies, as highlighted by the STAR*D study which suggests revisiting treatment adequacy.
- Genetic Testing: Advances in pharmacogenomics help personalize treatment by identifying genetic markers that predict medication responses, optimizing efficacy and reducing side effects.
- New Pharmacotherapy: Emerging treatments including psychedelics like ketamine and psilocybin offer new possibilities for rapid-acting antidepressant effects and are explored for their unique neurobiological targets.
- Role of Psychiatrists: Psychiatrists are crucial for tailoring treatments and supervising emerging therapies to ensure safe and effective management of TRD.