Sunday, April 21, 2024
Julie Myers, PsyD
Diagnosing Obsessive-Compulsive Disorder (OCD) can take years before individuals receive an accurate diagnosis. The average delay in diagnosis is 6 to 10 years from the onset of symptoms (Torres et al., 2018). One reason for this delay is the complexity of OCD symptoms, which can vary widely in severity and presentation, making it challenging for clinicians to recognize. Additionally, many individuals with OCD may feel embarrassed about their symptoms, leading them to conceal their struggles.
Mary recently sought us out for “treatment resistant depression” after decades of medication and psychotherapy failure. After a thorough assessment, Mary learned that she had OCD, which had gone unrecognized by dozens of providers. After receiving medications targeted to the OCD and EPR therapy, Mary has shown improvements in almost every domain of her life, including her depression.
Depression commonly co-occurs with OCD, further complicating the diagnostic process. Research suggests that up to two-thirds of individuals with OCD experience comorbid depression at some point during their illness (Pallanti et al., 2011). The presence of depressive symptoms can overshadow the OCD symptoms and lead clinicians to focus solely on treating depression, delaying the identification of underlying OCD.
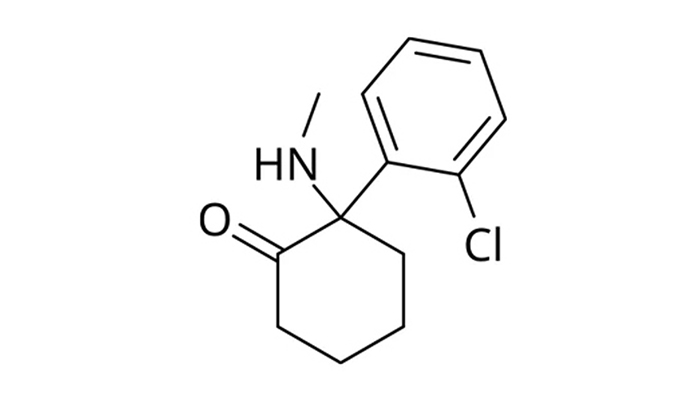
Treatment for OCD commonly involves Exposure and Response Prevention (ERP) plus selective serotonin reuptake inhibitors (SSRIs). For patients who don’t respond adequately to SSRIs, off-label medications such as memantine, naltrexone, or neuroleptics (e.g. aripiprazole) may be added. Treating the co-occurring depression is essential, as it not only compounds the burden of OCD but can also impair treatment response. SSRIs serve a dual role in this capacity, targeting both OCD and depressive symptoms (Pittenger et al., 2015).
Ketamine has shown promise in treating OCD. Studies have shown that ketamine therapy can lead to significant reductions in OCD severity, particularly in treatment-resistant cases (Bloch et al. 2012). A preliminary study presented at the Ketamine Conference in Oxford found that ketamine rapidly reduced the severity of OCD symptoms compared to placebo, and the effects of a single treatment were sustained for 3 weeks (van Roessel, 2024). While the precise mechanisms underlying ketamine’s therapeutic effects in OCD are still being studied, its ability to modulate glutamate neurotransmission and promote neuroplasticity may contribute to its efficacy. Incorporating ketamine treatment into comprehensive OCD management plans may offer hope for individuals who have not responded to traditional therapies.
Key Points
• Diagnosing OCD often faces delays of 6 to 10 years due to symptom complexity and stigma.
• Depression commonly co-occurs with OCD, complicating its recognition and treatment.
• SSRIs are primary for OCD treatment, with alternatives like memantine and aripiprazole used for non-responders.
• Ketamine shows promise in rapidly reducing severe OCD symptoms, especially in resistant cases.
You can learn more about what OCD and where to get help at the OCD International Foundation.