Monday, May 27, 2024
Alexander Papp, MD and Julie Myers, PsyD, MSCP
Introduction
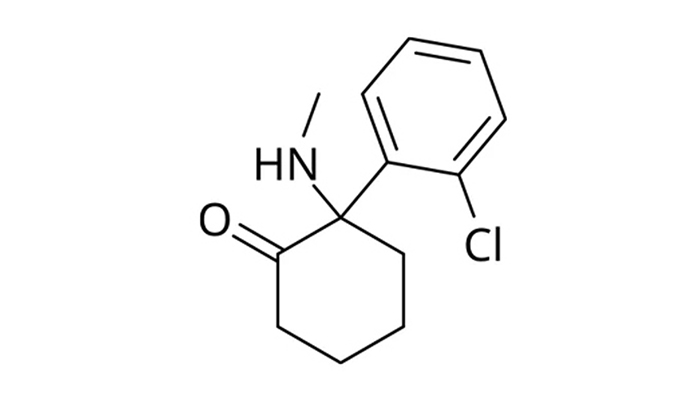
Recent clinical studies have explored the effectiveness of ketamine compared to traditional antidepressants in treating depression. Research indicates that traditional antidepressants lead to remission—defined as the complete disappearance of depressive symptoms—in approximately 30-40% of patients following one treatment cycle. In contrast, ketamine shows a significantly higher remission rate of 50-75%.
Moreover, the timeframe to achieve remission differs notably between the two treatments. Traditional antidepressants typically require 4-6 weeks to start showing effect, whereas ketamine can produce results in just a few days to a maximum of two weeks.
Qualitative Differences in Patient Experience
Beyond statistical outcomes, the qualitative difference in symptom improvement between these treatments is striking yet can be challenging to quantify (see e.g., Griffiths 2021). To better illustrate this, consider the experiences of two of our patients, Annie and Bella, who have undergone both traditional and ketamine treatments.
Annie’s Experience: A Shift from Shielding to Shelter
Annie, a 39-year-old woman, struggled with persistent depression since her postpartum period seven years ago. Traditional antidepressants provided partial relief but never full remission. Her experience with ketamine was profoundly different, achieving complete remission by the third treatment, which occurred over seven days. After six sessions, she was able to reduce her treatment frequency to once every six weeks.
Reflecting on her treatment, Annie shared, “The difference is not just that I feel better, but how I feel better. Being on an antidepressant felt like shielding my eyes from the sun with my hand—constantly adjusting to find relief. Ketamine, on the other hand, is like sitting under a wide umbrella. It allows me to relax fully without constant adjustment.”
Bella’s Experience: From Mud to Gentle Rain
Bella, a 55-year-old scientist, initially faced challenges with ketamine due to her logical mindset and significant psychological trauma. Traditional antidepressants caused her to gain weight and had unpleasant side effects like brain zaps if she missed a dose. Initially, her response to ketamine was subdued, with minimal improvement up to her sixth treatment.
However, she noticed a significant uplift in her mood days after her last session, prompting her to continue treatment. Bella described her experience as, “Taking traditional medication was like wading through mud—constantly struggling to stay clean. Ketamine, however, felt like walking in gentle rain; any mud simply washes away.”
Conclusion: The Effortlessness of Maintaining a Better Mood
Both cases highlight a common theme: The ease of maintaining an improved mood with ketamine compared to traditional antidepressants. These patient stories are invaluable, as they underscore the significant impact of ketamine on our patients’ lives and their mental health.
At our clinic, we find it immensely rewarding to witness such positive responses to treatment and are deeply appreciative of our patients who share their personal experiences with us.
References:
1. Griffiths, C., Walker, K., Reid, I., da Silva, K.M. and O’Neill-Kerr, A., 2021. A qualitative study of patients’ experience of ketamine treatment for depression: The ‘Ketamine and me’ project. Journal of Affective Disorders Reports, 4, 100079. https://dx.doi.org/10.1016/j.jadr.2021.100079
2. Strasburger SE, Bhimani PM, Kaabe JH, Krysiak JT, Nanchanatt DL, Nguyen TN, Pough KA, Prince TA, Ramsey NS, Savsani KH, Scandlen L, Cavaretta MJ, Raffa RB. What is the mechanism of Ketamine’s rapid-onset antidepressant effect? A concise overview of the surprisingly large number of possibilities. J Clin Pharm Ther. 2017 Apr;42(2):147-154. doi: 10.1111/jcpt.12497. Epub 2017 Jan 22. PMID: 28111761.
3. Hasselmann HW. Ketamine as antidepressant? Current state and future perspectives. Curr Neuropharmacol. 2014 Jan;12(1):57-70. doi: 10.2174/1570159X113119990043. PMID: 24533016; PMCID: PMC3915350.