Sunday, January 28, 2024
Alexander Papp, MD and Julie Myers, PsyD, MSCP
Introduction
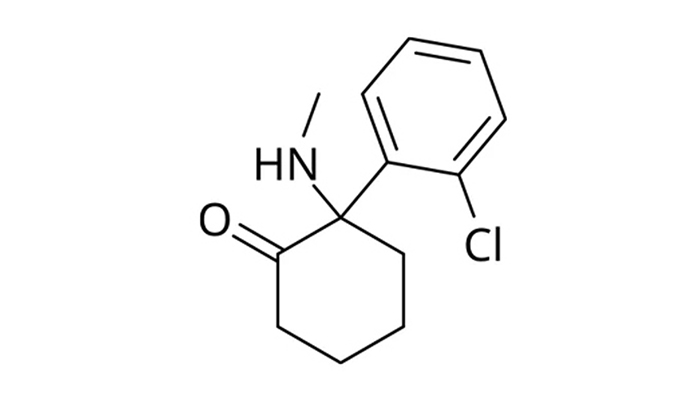
Ketamine, an NMDA receptor antagonist, has shown promise in the treatment of various psychiatric disorders, including depression and PTSD. Its rapid-acting therapeutic effects have made it an appealing option in clinical settings under strict supervision. However, the trend towards take-home ketamine, facilitated through prescriptions for nasal sprays and oral lozenges, raises significant safety and efficacy concerns. This blog entry explores some of the reasons why take-home ketamine may not be a suitable option for many patients, citing current research and clinical guidelines.
Risk of Abuse and Misuse
One of the primary concerns with take-home ketamine is the potential for abuse and misuse. Ketamine is classified as a Schedule III controlled substance in the United States due to its potential for abuse and dependency. The drug’s dissociative effects, which can be pleasurable or euphoric, might lead to its misuse. Individuals with a history of substance use disorders may be particularly at risk (Morgan & Curran, 2012).
Challenges in Monitoring Side Effects
Ketamine’s side effects, which include dissociation, confusion, and in some cases, increased blood pressure and euphoria, require careful monitoring. In a clinical setting, healthcare providers can immediately address these effects, adjust doses, and provide support. In a home setting, this level of monitoring is not possible, potentially leading to unchecked side effects and complications (Andrade, 2017).
Dosing Issues
Proper dosing of ketamine is critical to its effectiveness and safety. In a clinical setting, doses are carefully controlled and administered based on a patient’s response to treatment. At home, patients may not adhere strictly to prescribed doses, either intentionally or accidentally, leading to under-dosing (ineffectiveness) or overdosing (safety risks).
Lack of Long-Term Safety Data
Ketamine’s long-term effects are still not well-understood, especially regarding chronic use outside of controlled clinical environments. There is a paucity of data on the outcomes of prolonged, unsupervised ketamine use, which is concerning given the drug’s complex effects on different organ systems, including the central nervous system and bladder (Correia-Melo et al., 2020).
Legal and Ethical Concerns
Prescribing take-home ketamine also introduces legal and ethical challenges. Given its status as a controlled substance, the prescription, distribution, and management of take-home ketamine must adhere to stringent regulatory standards. Physicians prescribing ketamine for home use face potential legal liabilities should adverse effects occur, adding another layer of complexity to its use.
The Role of the FDA
In April 2023, the FDA received an adverse event report of a patient who experienced respiratory depression after taking compounded oral ketamine outside of a health care setting for the treatment of PTSD. The patient’s ketamine blood level appeared to be twice the blood level typically obtained for anesthesia. This event predates the death of Matthew Perry, but in a way it might have foreshadowed it. The FDA encourages compounders, patients, and health care providers to report adverse events associated with compounded ketamine products to its MedWatch Adverse Event Reporting program.
Conclusion
While ketamine offers significant benefits in the treatment of certain psychiatric conditions, the risks associated with take-home use are considerable. Without the safeguards of controlled administration and professional monitoring, the potential for abuse, adverse effects, and other complications increase markedly. For these reasons, ketamine treatment should remain a supervised medical procedure until more comprehensive data can support the safety and efficacy of at-home use.
References
- Morgan, C. J. A., & Curran, H. V. (2012). Ketamine use: A review. Addiction, 107(1), 27-38.
- Andrade, C. (2017). Ketamine for Depression, 6: Effects on Suicidal Ideation and Possible Use in Suicide Prevention. The Journal of Clinical Psychiatry, 78(8), e1049-e1052.
- Correia-Melo, F. S., et al. (2020). Safety and efficacy of ketamine in the treatment of mood disorders: A systematic review. Journal of Psychiatric Research, 123, 27-51.